All of Rice’s medical plan options cover prescription drugs through our Pharmacy Benefit Manager (PBM), Capital Rx.
Effective July 1, 2025
Starting July 1, 2025, Capital Rx, Rice's prescription manager, will transition from Optum to Costco Pharmacy for mail-order, specialty, and infusion services, bringing you an improved experience.
What services and programs are available to support your needs?
- Education and support programs to help manage your condition.
- Delivery to your home or another address within two days of ordering is at no cost.
- Highly trained pharmacists and nurses are available to answer any questions.
- Insurance specialists to help you get the most out of your benefits.
- Therapy-related ancillary medical supplies are provided at no additional cost.
What You Need to Know:
- Your existing prescriptions will be securely transferred to Costco Pharmacy if you have refills available.
- See the resources below for instructions on accessing your new online pharmacy account.
Visit these resources for more information.
Getting Started
To access pharmacy benefits, employees should provide their Aetna ID card to the pharmacist and direct the pharmacist to the information on the back of the card. The Aetna ID number is also the pharmacy ID number. If an employee has not received their Aetna ID card or only printed the front, the necessary information is listed below.

Formulary Tiers
There is a new formulary with Capital Rx. A “formulary” is a list of medications organized into groups or “Tiers.” Please review this information and discuss any potential cost increase with your doctor. They may agree to move you to a lower-cost alternative.
Formulary Tier Definitions
|
Tier One (1) |
Most Generics |
|
Tier Two (2) |
Preferred (also called formulary) medications. These are on the preferred medications list. |
| Tier Three (3) |
Non Preferred medications not on the preferred list |
|
Tier Four (4) |
Specialty Medications |
For the most accurate information about all medication coverage, employees should register and log on to cap-rx.com. Use the "Find Best Price” tool to determine the drug's tier and how much it will cost. Capital Rx customer service representatives are also available at (833) 502-1307.
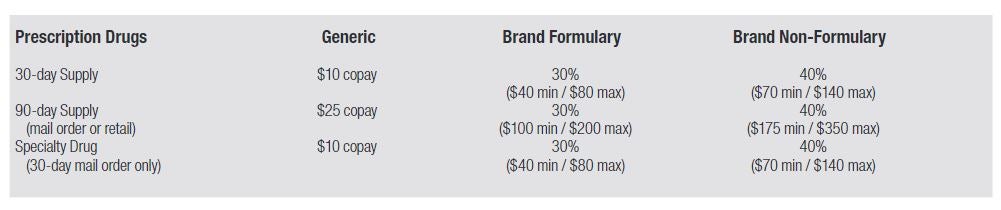
Copays and Coinsurance
Copays and coinsurance, the portion of the drug cost you are responsible for paying, are listed for all medical plans in the table below.
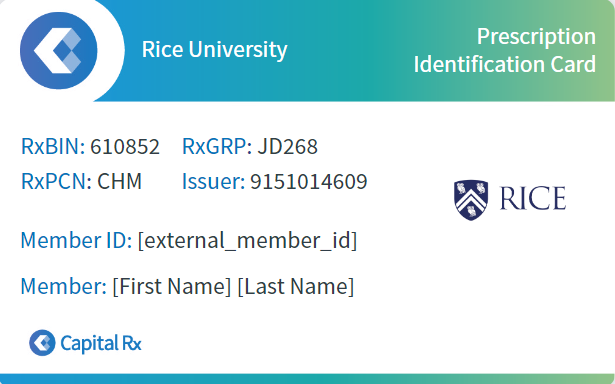
Identification Cards
Your prescription drug information can be found on the back of your Aetna ID card. You can download or print a Capital Rx ID card anytime from their website or app. Should you misplace your ID card and you need your covered prescriptions immediately, please take the following information (along with the Aetna temporary ID) to the pharmacy and present it to the pharmacist:
- BIN: 610852
- PCN: CHM
- Rx Group Number: JD268
If you have problems with your prescription claim, please ask the pharmacist to contact the Capital Rx at (833) 502-1307 or your benefits team.
Retail Services
The Capital Rx's network includes over 60,000+ retail locations representing all major chains and many independent pharmacies throughout the United States. Present your Aetna ID card (with Capital Rx information on the back) and your prescription to a participating pharmacy. Visit this link to view a list of National Chain Pharmacies.
Benefits are available only through a network pharmacy. If your pharmacy is not in the network, you can submit a request to add that pharmacy to the network through the benefits department at benefits@rice.edu.
At the time of service, you must pay the required copayment or coinsurance (your portion of the cost of the medication), or if you are on the High Deductible plan, your deductible and then your copayment. To access a Pharmacy Locator, please log into cap-rx.com. Select "Find a Pharmacy" under the "Prescriptions" menu. You may also call Capital Rxs customer service representatives at (833) 502-1307.
- Dispense as Written
-
Dispense, as written, requires that if a generic drug is available for your prescription, the prescription will be filled with the generic. If you request the brand, you will be charged both the difference in the actual cost of the generic and brand name drug and the brand name copay. If it is medically necessary for you to use the brand name medication, your doctor may specify that request by:
Writing for the brand name and writing "dispense as written."
If these two criteria are met, you will pay the applicable brand copay only.
- Maintenance Medications
-
Maintenance drugs are medications prescribed for chronic, long-term conditions and are taken on a regular, recurring basis. Examples of chronic conditions that may require maintenance drugs are high blood pressure, high cholesterol, and diabetes. Your pharmacist will inform you when the plan requires you to purchase your maintenance medication at 90 days.
For convenience and so that you can be sure that your medication and dosage are appropriate for new prescriptions, you may fill a 30-day prescription up to two times at a retail pharmacy. After that, maintenance medications must be filled using 90-day supplies. You can do this at a retail pharmacy or use the mail-order program through Capital Rx. Be sure to ask your doctor for a 90-day prescription with the appropriate number of refills for your maintenance drugs.
- Previous Mail Order, Specialty, and Infusion Services Provider
-
Starting July 1, 2025, Capital Rx, Rice's prescription manager, will transition from Optum to Costco Pharmacy for mail-order, specialty, and infusion services.
If you need to contact Optum for a previous prescription prior to the transition for any mail-order services, call (833) 502-1307. Follow the prompts for "medications delivered to your home.)
For more information, please visit the Optum Home Delivery FAQs.
- Mail Order Services
-
Starting July 1, 2025, Capital Rx, Rice's prescription manager, will transition from Optum to Costco Pharmacy for mail-order, specialty, and infusion services, bringing you an improved experience.
What services and programs are available to support your needs?
- Education and support programs to help manage your condition.
- Delivery to your home or another address within two days of ordering is at no cost.
- Highly trained pharmacists and nurses are available to answer any questions.
- Insurance specialists to help you get the most out of your benefits.
- Therapy-related ancillary medical supplies are provided at no additional cost.
What You Need to Know:
- Your existing prescriptions will be securely transferred to Costco Pharmacy if you have refills available.
- See the resources below for instructions on accessing your new online pharmacy account.
Costco Mail Order Pharmacy can be contacted at 1-800-607-6861, Mon-Fri 5 am-7 pm PT or Sat 9:30 am - 2 pm PT. Fax number is 1-800-633-0334.
Visit these resources for more information.
- Step Therapy
-
Step Therapy means ensuring you get safe, effective medicine for your condition at the lowest possible cost for you and for Rice.
Often, several different medications can be used to treat a condition. Step therapy requires you to try the ones that are lower cost, often generics first, to see if they work for you. This is step one. If step one does not work, then step two medicine can be tried. Depending on the medication, there can be several steps before you are approved for the medication originally written, and often, a step one or two medication works well to treat a given condition, making the more expensive medication unnecessary.
- Specialty Medications
-
Specialty medications are often high-cost and require special handling (for example, they may need refrigeration). Costco Pharmacy can only dispense these medications for a 30-day supply. Here is the link to the current specialty drug listing.
In addition, some specialty medications may have drug manufacturer copay assistance programs. Participation in these programs is optional, but you may enroll and contact Costco to apply these funds toward your Rice copayment. Often, using these programs can reduce your copayment to $0. The best way to contact Costco is to call Capital Rx at (833) 502-1307 and select the specialty medication option in the telephonic menu.
Visit these resources for more information.
Prior Authorization
Keeping your medications safer and more affordable is a priority for our pharmacy program. That is why your pharmacist may tell you that prior authorization is required when prescribing certain medications. This means that Capital Rx needs more information to make sure the prescribed medicine will work well for you and your condition, and that the plan covers it.
Only your doctor can provide the necessary information for prior authorization. There are several ways to do this.
- Your doctor can call (833) 502-1307 and provide the necessary information over the phone.
- Your doctor can provide the needed information online with Capital Rx.
- You can call (833) 502-1307 with your doctor's name, address, fax number, and phone number and request that Capital Rx reach out to your doctor to request the needed information.
Prescription FAQ’s
- How do I create an account, and who do I contact for help?
-
To create an account, please visit cap-rx.com (click on the "Member Portal" button and click the "Don't have an account? Register Now" link to register). You can also download the Capital Rx app (called "Capital Rx Pharmacy..." in the app stores).
Additional guidance can be found below:
Capital Rx Customer Service can be contacted at (833) 502-1307 for further assistance.
- How does the 90-day retail prescription drug program work?
-
The medical plan provides for the purchase of 90-day maintenance prescriptions at retail pharmacies that accept Capital Rx coverage, which includes all of the major pharmacy and supermarket chains in the United States. You will pay for the 90-day prescription (at 2.5 times the 30-day cost) and receive the full 90-day supply in one transaction. As with a 30-day prescription, it is possible that the pharmacy may run out of medication, but if that happens, they will send you home with the quantity they have in stock, and you will be able to pick up the remainder of the order when the pharmacy re-stocks the medication, usually within a day or so. Both retail pharmacy and mail order services are available to fill your 90-day prescriptions.
Retail pharmacies will fill maintenance prescriptions of 30 days for two one-month cycles; thereafter, you must begin to purchase maintenance drugs in 90-day increments.
- What is a maintenance medication? How will I know if I am required to get a 90-day supply?
-
Maintenance drugs are medications prescribed for chronic, long-term conditions and are taken on a regular, recurring basis. Examples of chronic conditions that may require maintenance drugs are high blood pressure, high cholesterol, and diabetes. Your pharmacist will inform you when the plan requires you to purchase your maintenance medication at 90 days, or you can call Capital Rx at (833) 502-1307, and they can tell you if your medication requires a 90-day fill.
- Will some generic drugs for chronic conditions still be covered at $0 copays, even though I order a 90-day supply?
-
Yes, generic medications for certain chronic conditions are covered for a $0 copay, even for 90-day orders. As part of our plan’s effort to help employees manage certain long-term medical conditions, certain generic drugs used to control high blood pressure, cholesterol, diabetes, and asthma will remain available for the $0 copay. The Affordable Care Act includes these conditions and the option to offer them at $0 copayment.
- Why is the pharmacy declining my Aetna benefits coverage for my medication?
-
Capital Rx is Rice’s pharmacy benefits manager. Please refer your pharmacist to the information on the back of your Aetna card.
90-day fills are required for maintenance medications after two 30-day fills have been dispensed. Your doctor will have to update your prescription to 90 days in order for your medication to be dispensed and paid for by the plan.
- Please explain Dispense As Written.
-
Rice's dispensing as written requirement provides that if your physician writes for a brand drug and a generic is available, your prescription will be filled with the generic. If you request a brand drug instead of the generic, you will be charged both the difference in the actual cost of the generic and brand name drug and the brand name copay. If your physician determines that it is medically necessary for you to use a brand drug, he or she can write a prescription that includes 1) the brand name prescribed and 2) directions to “dispense as written,” and you will be able to purchase the drug for the applicable brand copay.
Please contact us if you have other questions. Call 713-348-2363 (BENE) or email us at benefits@rice.edu.
